Dr Jenny Spiga
Lecturer – Physics
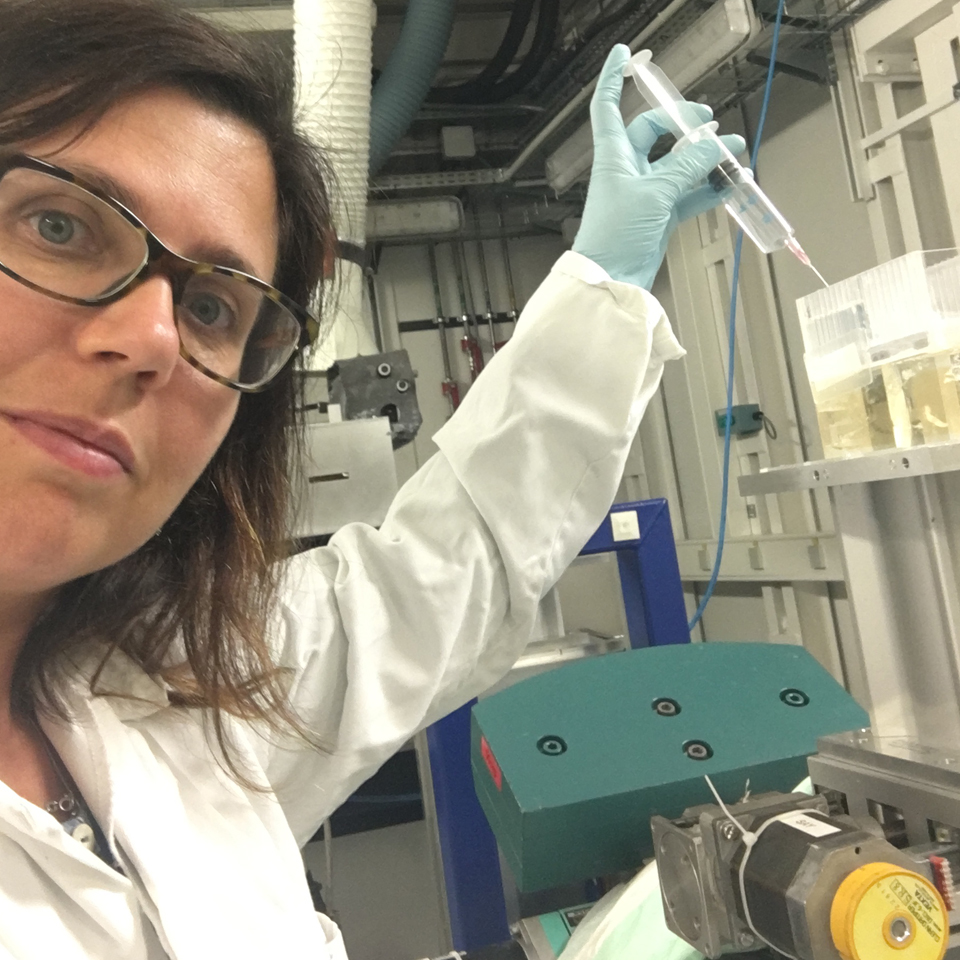
Jenny Spiga is a Medical Physicist who explores new healthcare technologies. She uses computational modelling and experimental methods to investigate innovative x-ray radiotherapy techniques to improve cancer treatment, including Microbeam Radiation Therapy (FLASH-MRT). Over the years, she has been awarded funding from a range of sources to support her groundbreaking research. She is a member of the Global Challenge Network+ in Advanced Radiotherapy which brings together clinical and academic researchers in radiotherapy to accelerate patient benefit.
Developing a new approach to cancer treatment
Cancer is treated in several ways, including radiation therapy (aka radiotherapy) which uses x-rays or particle beams to destroy malignant cells. It can be very effective at slowing and even curing cancer – but does cause some side effects and can damage healthy tissue around the treated area. Microbeam Radiation Therapy (MRT) is an emerging technique that targets tumours more effectively, reducing harm to healthy cells. Jenny is among a few scientists worldwide, working to refine MRT so that, one day, it can be used to save lives.
I’ve always been curious – and love combining ideas from different disciplines to solve problems. Medical physics appealed to me, from the very start, because of the positive impact it can have on people's lives.
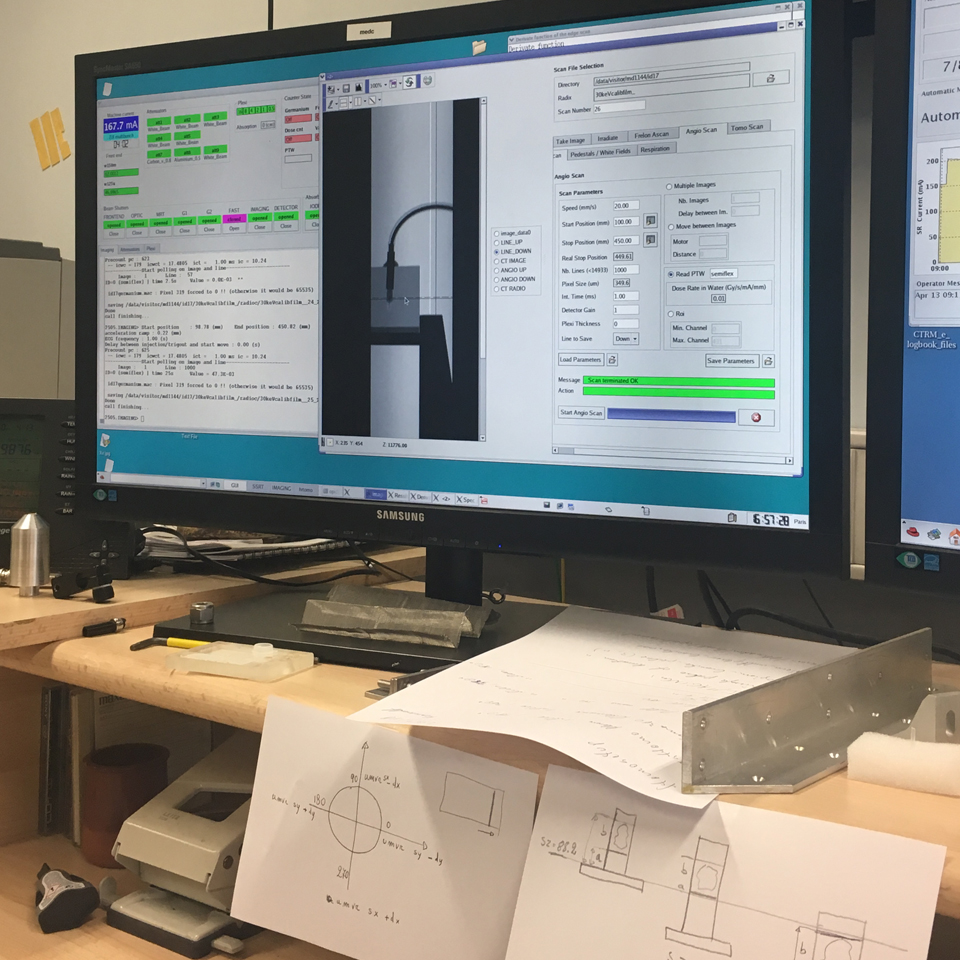
My research interests lie in dosimetry (radiation dosage), Monte Carlo simulations (a modelling technique) and the experimental development of new radiation therapies that employ the latest x-ray sources.
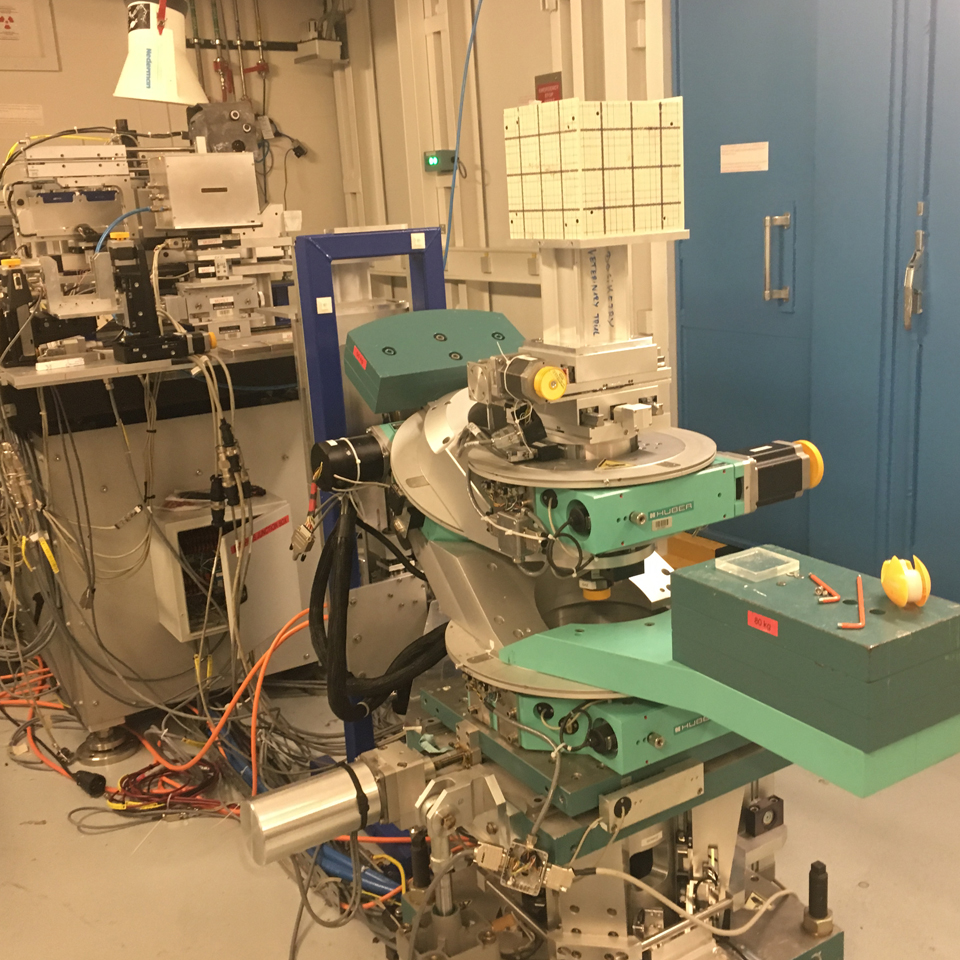
I collaborate with the biomedical group ID17 at the European Synchrotron Radiation Facility (ESRF, Grenoble).
Preclinical studies are really very promising, suggesting that MRT could be an effective tool in our ongoing fight against cancer.
I’ve worked with them for many years, contributing to several peer reviewed research papers – mostly about MRT – and working on the application of x-ray microbeams in the treatment of epilepsy.
So, what is MRT? It’s actually a relatively recent discovery. Developed at several research centres worldwide – including the ESRF – it uses synchrotron radiation to fight cancer.
By delivering the radiation in a very narrow array of beams – rather than the usual single wide beam of conventional radiotherapy – it greatly reduces the risk of damage to the patient’s healthy tissue.
Preclinical studies are really very promising, suggesting that MRT could be an effective tool in our ongoing fight against cancer – and it’s well suited for treating areas where minimal collateral damage is essential, such as the brain.
My contribution to MRT’s development is to determine the optimal dose profiles that maximise its therapeutic benefit with little or no harm to healthy tissue.
One of the major obstacles in bringing MRT to clinical practice is cost. Another is the sheer size of a synchrotron – some are about 1km in diameter! How could one of these colossal machines possibly be housed at a hospital?
Therefore, another area I’m exploring is compact alternatives to a synchrotron that can effectively deliver MRT - taking the technique from lab to clinical trials and, eventually, the treatment room.
Here at Loughborough, I am continuing my work on MRT - exploring potential alternative sources.
Using mathematical models and high-performance computers, my aim is to determine the amount and rate at which these new sources can deliver radiation to the body.
Developing a new treatment for cancer is hugely exciting - and a great motivator first thing on a Monday morning!
My research journey
I studied in my hometown – at the University of Cagliari – on the beautiful island of Sardinia. From an early age, I knew I wanted to pursue something mathematical, but ventured into Physics almost by accident.
My decision probably had a lot to do with my wonderful and inspiring Physics teacher at secondary school. They introduced me to the subject’s many applications, and regularly assigned me additional topics to explore. So, I guess I unwittingly started my research journey right back then.
Plus, I had a fabulous calculator that I loved and wanted to put through its paces…
As an undergraduate, I was awarded an Erasmus bursary to work at the ESRF where I had access to the ID17 biomedical beamline. A dream come true for someone focusing on radiotherapy.
At that time, my Mum had been diagnosed with a breast tumour. So, I was drawn to this area of research for personal as well as academic reasons.
I’ve actually spent three spells at the ESRF. It’s where I learned to run simulations – something that has proved very useful over the years.
In 2011, I embarked on a new journey. I moved to the UK, got married and started my family – taking a career break to focus on my new adventure as a Mum.
However, I did miss my research. In 2017, I decided to return to academic life, and was delighted to secure a fantastic opportunity – a Daphne Jackson Fellowship at the University of Warwick where I stayed for six years, teaching and continuing my research.
The DJT Fellowship is more than a grant, it’s a community full of people who share similar stories and a great team of mentors.
Warwick provided me with so many opportunities and new experiences – including teaching and outreach projects promoting women in science. I’m a passionate advocate for inclusion, actively encouraging people from all backgrounds to follow careers in STEM fields.
To this end, I’m a member of the International Network of Women Engineers and Scientists (INWES) and I collaborate in international diversity and inclusion projects, together with the University of Warwick and INWES.
I joined Loughborough in 2023 and work with an incredible team of people with whom I’ve established the Applied Radiation and Medical Physics Group (ARAMP). I co-lead ARAMP with Sarah Bugby and Fasil Kidane Dejene. Working with researchers, clinicians and industry partners worldwide, we are developing new techniques to solve societal challenges and improve patient care.
The best part of my research lies in collaborating with diverse international colleagues to create meaningful impacts on people's lives. Moving forward, I hope to help accelerate MRT research, facilitating its transition from the laboratory to hospitals – ultimately benefitting everyone worldwide.
